Abstract
Introduction
WHIM syndrome (WHIMs) is a rare disorder caused by germline CXCR4 mutations, classically characterized by warts, hypogammaglobulinemia, infection, and neutrophil retention in the bone marrow (BM), with distinctive morphology termed myelokathexis. Demonstration of myelokathexis by BM evaluation plays a key role in disease recognition and diagnosis. However, the spectrum of BM morphologic features and correlation with specific CXCR4 mutations are not well described. Moreover, diagnostically useful peripheral blood (PB) smear findings and morphologic changes after CXCR4 antagonist therapy are largely unknown.
Methods
We conducted a multinational, retrospective review of clinicopathologic features of patients with established WHIMs (n=20) or germline CXCR4 variants considered likely pathogenic or of uncertain significance (n=3), including 14 BM specimens and 10 PB smears. Assessments to date were performed by 2 observers in 6 cases and a single observer in the remainder. BM morphology was compared to other neutropenia disorders (Shwachman-Diamond syndrome, n=5; GATA2 deficiency, n=5; severe congenital neutropenia with ELANE variants, n=4) and patients without hematologic disorders (n=10), together "controls." Correlations and contingency analysis (2-tailed Fisher exact test) were performed using Prism v.9.4.0 (GraphPad Software).
Results
Median age at WHIMs diagnosis was 18.5 years (range, 0.1-53 years), with female:male ratio of 1.1:1. Recurrent infections, warts, and hypogammaglobulinemia were present in 100%, 53%, and 40% of cases, respectively.
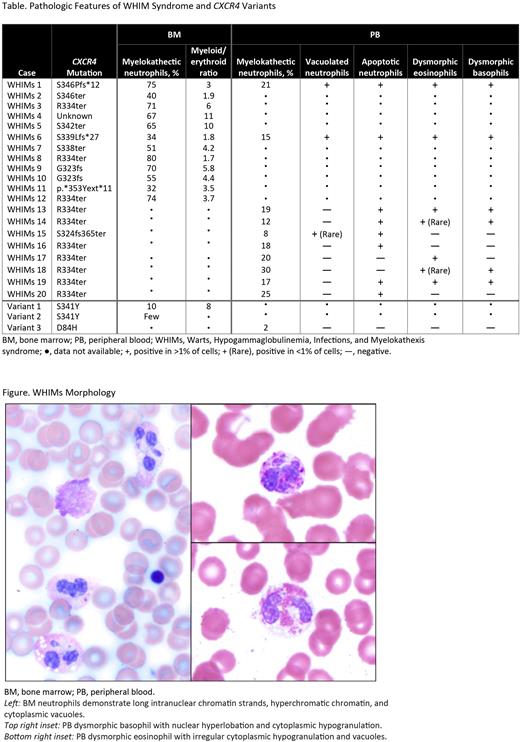
BM aspirate smears contained neutrophils with long intranuclear chromatin strands and hypermature condensed chromatin ("myelokathectic neutrophils") in all WHIMs cases, making up 32% to 80% (median 66%) of total neutrophils (Table). In comparison, neutrophils with myelokathectic changes were seen in 0% to 4% of control BMs. Myeloid hyperplasia (myeloid:erythroid ratio >4:1) was present in 50% of WHIMs and 4% of controls (P=.0028); vacuolated neutrophils in 92% of WHIMs (≤29% of total neutrophils) and 17% of controls (P<.0001); apoptotic neutrophils in 58% of WHIMs (1%-4% of total neutrophils) and 8% of controls (P=.0025); and nonparatrabecular neutrophil clusters on core biopsy in 3/3 WHIMs and 5% of controls (P=.0017). Vacuolated eosinophils and myeloid shift toward hypermaturity were present in WHIMs. There was no correlation between percentage of BM myelokathectic neutrophils and degree of CXCR4 truncation. BM in 2 patients with CXCR4 p.S341Y showed myeloid hyperplasia, increased neutrophil apoptosis, and infrequent myelokathectic neutrophils (5%-10%).
Neutropenia was present in all untreated WHIMs. Myelokathectic neutrophils were present in PB of all patients with known WHIMs and accounted for 8% to 30% (median, 18%) of total neutrophils. Percentage of PB myelokathectic neutrophils showed an inverse correlation with absolute neutrophil count (ANC) (r=-0.783; P=.0074). Neutrophil apoptosis, neutrophil vacuolization, dysmorphic (hypogranular, hyperlobated, vacuolated, or apoptotic) eosinophils, and/or dysmorphic basophils were present in 80%, 30%, 70%, and 60% of WHIMs cases, respectively (Figure). PB in 1 patient with
CXCR4p.D84H showed neutrophil hypolobation without myelokathectic morphology. CXCR4 antagonist therapy with plerixafor (n=4) [Dale et al. Blood. 2011] or mavorixafor (n=1) (interval, 4-12 h) resulted in increased white blood cell (WBC) count and ANC, with a similar proportion of myelokathectic neutrophils as before therapy.
Conclusions
In WHIMs BM specimens, the proportion of myelokathectic neutrophils is variable and may not be prominent; the classic finding of myeloid hyperplasia is only present in a subset of cases, which may result in underrecognition of the disease and delayed diagnosis. Neutrophil vacuolization and apoptosis, eosinophil vacuolization, and prominent neutrophil clusters may also prompt disease recognition. We establish characteristic PB morphologic features which, in a patient with unexplained neutropenia, may suggest a diagnosis of WHIMs, including myelokathectic neutrophils, neutrophil vacuolization or apoptosis, and dysmorphic eosinophils and basophils. CXCR4 antagonist therapy led to an increase of WBC/ANC, while pretreatment morphologic changes persisted after a short interval. Analysis of additional cases is ongoing.
Disclosures
Kelley:X4 Pharmaceuticals, Inc.: Research Funding. Neff:EUSA Pharma: Consultancy, Speakers Bureau; Abbvie: Consultancy; Guidepoint Global: Consultancy. Yilmaz:X4 Pharmaceuticals, Inc.: Research Funding. Neri:X4 Pharmaceuticals, Inc.: Current Employment, Current equity holder in publicly-traded company. Walter:Pharmig: Membership on an entity's Board of Directors or advisory committees; UptoDate: Other: Medical Writer; Regeneron: Consultancy; Enzyvant: Consultancy; Grifols: Consultancy; CSL-Behring: Consultancy; X4 Pharmaceuticals, Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees; Octapharma: Research Funding; ADMA Biologicals: Consultancy; MustangBio: Research Funding; Chiesi: Research Funding; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Tarrant:US Department of Justice: Consultancy; X4 Pharmaceuticals, Inc.: Research Funding; Abbvie: Research Funding; Viela Bio: Research Funding; Pfizer: Honoraria. Bolyard:X4 Pharmaceuticals, Inc.: Research Funding. Sockel:Novartis: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Active Biotech: Research Funding; Gilead: Honoraria; SOBI: Honoraria. Newburger:X4 Pharmaceuticals, Inc.: Consultancy; UpToDate: Patents & Royalties: Section Editor. Dale:X4 Pharmaceuticals, Inc.: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal